Co-designing Sustainable Cardiac Neurodevelopmental Models of Care for Children with CHD
By Karen Eagleson, Clinical Nurse Consultant, CHD LIFE Program
Children’s Health Queensland Hospital and Health Service

Congenital heart disease (CHD) is one of the most common conditions for children to be born with, affecting approximately one in a hundred live births. Children with CHD and their families can face many challenges, from time of diagnosis, through surgeries, and changes in their health as they grow up. Thankfully, with advances in cardiac surgery and care, most children with CHD are surviving into adulthood. In fact, there are now more adults living with CHD than children.
But there is much more to life than survival. Whilst most children with CHD will develop and function similarly to their peers, others will experience challenges. This is for a range of reasons including clinical, genetic, and sociodemographic factors that are yet to be fully understood. Challenges can be mild but across multiple developmental areas, with new issues emerging over time. This can impact children with CHD reaching their potential.
Subsequently, long-term developmental follow-up is recommended for children with CHD at high-risk for challenges. Best practice recommendations have been developed in the United States, as well as developmental follow-up programs, also predominantly US based. Informed by these, in 2013 the Queensland Paediatric Cardiac Service partnered with the local Child Development Service to establish a pilot program – now known as CHD LIFE (Long-term Improvement in Functional hEalth) – based at the surgical centre. Grant funding through HeartKids, the national CHD advocacy group, was an important factor in getting our program underway. However, consistent with recently reported experiences of other CHD developmental follow-up endeavours in public health system contexts, we faced significant challenges to the sustainability and desired growth of our program.
In 2016 we extended our partnerships, undertaking a project with the Queensland Child and Youth Clinical Network to develop a more sustainable, family-centred approach to developmental follow-up care for high-risk children with CHD across Queensland. We engaged with primary, secondary and tertiary health services statewide, as well as families and young people living with CHD to develop a care pathway to support accessing developmental follow-up close to home. We also established a database to collect outcome and service access data to enable us to continue to understand and improve care.
The next important step in the CHD LIFE journey is CHD LIFE+. Led by AusHSI, and in partnership with cardiac centres nationally, developmental follow-up experts, HeartKids and Children’s Hospital Foundation, this program of research (2020-2024) aims to develop family-centred, long-term developmental care models across Australia, including evaluation of our CHD LIFE model. Funded by the Medical Research Future Fund, this project will align with the Standards of Care for Childhood-onset Heart Disease where neurodevelopment is a focus area.
We have learned a lot throughout our CHD LIFE work, including the critical value of partnerships. Health care services, advocacy groups and families, and academic partners can bring together an incredible wealth of knowledge and experience to develop innovative approaches and improvements in care. With neurodevelopment a national priority in the care of children with CHD, strong partnerships are more important than ever.
IMAGES
TOP (L-R): Karen Eagleson, A/Prof Sanjeewa Kularatna, Dr Sameera Senanayake, Dr Ben Auld, A/Prof Rob Justo, Jenna English, Dr Bridget Abell, Prof Steven McPhail
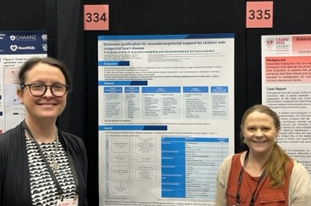
BOTTOM (L-R): Karen Eagleson, Dr Bridget Abell,